What Is Sleep Apnea?
Sleep apnea is a disorder in which a person stops breathing when they are asleep. It has been estimated that 1 in 3 men and 1 in 6 women are affected by some form of this condition.

At the St. Louis Sinus Center, Dr. James Gould is experienced in treating sleep apnea in the St. Louis and Festus, MO areas. Using state-of-the-art technology, he will assess your condition and work with you to develop a personalized treatment plan that fits your lifestyle.
What Are The Symptoms Of Sleep Apnea?
Most people recognize sleep apnea as loud, chronic snoring. However, there are other indicators that should not be overlooked. Symptoms of sleep apnea could include:
- Night sweats
- General lack of energy
- Poor concentration/brain fog
- Constant sleepiness
- Weight gain
- Sexual dysfunction
- Forgetfulness
- Frequent nighttime urination
It is believed that the symptoms of sleep apnea may present themselves more subtly in women. A woman affected by sleep apnea may be diagnosed with depression or anxiety, insomnia, or with side effects of menopause.
Types of Sleep Apnea
People generally get diagnosed with one of three main types of sleep apnea. These include:
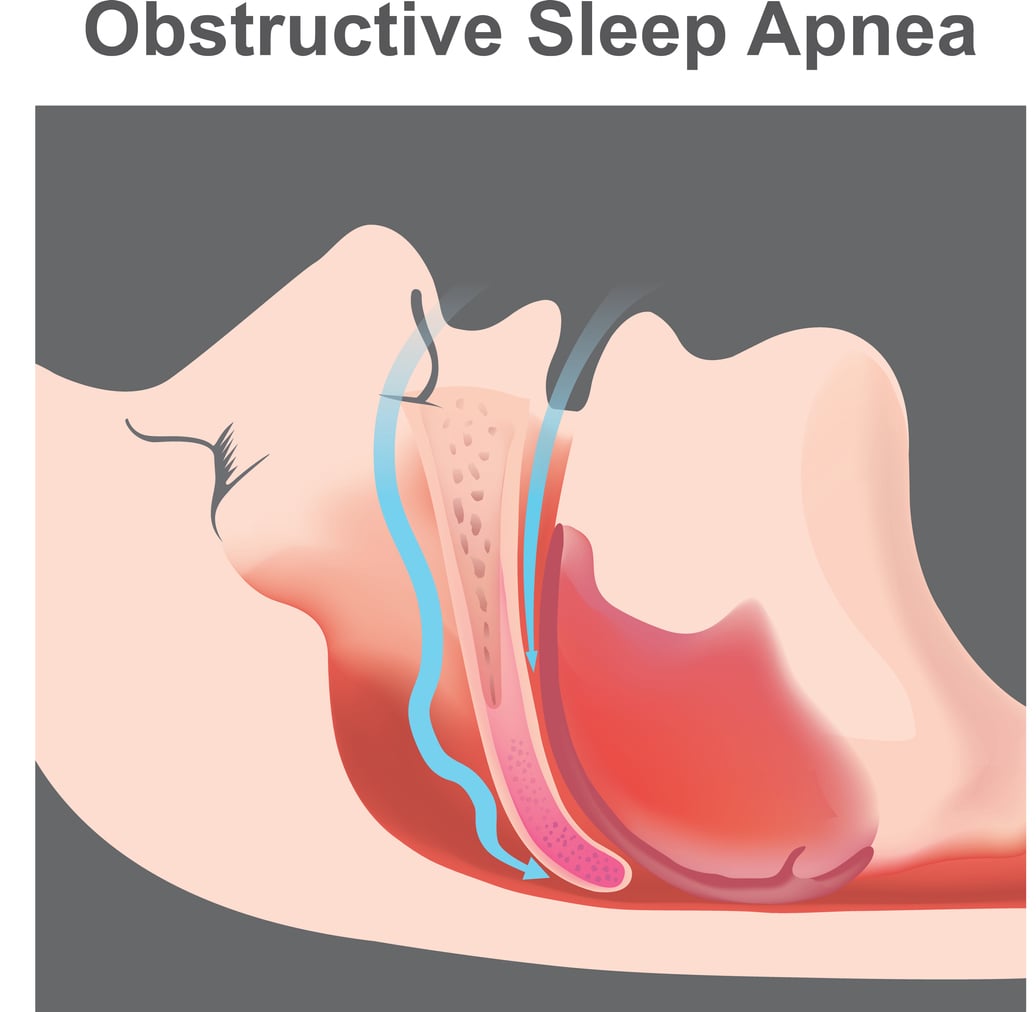
- Obstructive sleep apnea (OSA). This condition accounts for more than 80% of sleep apnea diagnoses. OSA occurs when the airway becomes obstructed by soft tissue.

- Central sleep apnea (CSA). This type of sleep apnea occurs when the brain does not signal the body to breathe. CSA is related to a malfunction in the central nervous system.
- Complex sleep apnea (CompSA). When obstructive sleep apnea and central sleep apnea combine, the condition is diagnosed as CompSA. This is a relatively rare sleep disorder.
Who Is Most Likely To Suffer From Sleep Apnea?
Research has identified several risk factors for sleep apnea. These include age, lifestyle, genetics, and ethnicity.
- Age. A person may develop sleep apnea at any age. However, the risk increases as we grow older. Researchers believe this is due in part to the way the brain controls breathing and how this function changes with age. Age-related fat accumulation around the neck could also explain this increase.
- Lifestyle. Alcohol alters the way the brain behaves during sleep. It also has a depressive effect, which could initially deepen a person’s state of sleep and the extent of muscle relaxation around the airway. Smoking can contribute to sleep apnea by causing inflammation in the upper airway. Finally, sleep apnea could be attributed to obesity caused by poor eating habits.
- Heredity. Studies in twins with sleep apnea suggest that a genetic component exists in the development of this condition. This relates to the structural development of the skull and face and the way in which the brain controls sleep functions.
- Ethnicity. Statistics show that Native Americans, Hispanics, and blacks are more commonly affected by sleep apnea than other ethnicities.
"Great staff! Clean and comfortable office. I highly recommend Dr. Gould."
How Do You Diagnose Sleep Apnea?
A multi-pronged approach is taken to diagnose sleep apnea. Your doctor will conduct a thorough medical history and health examination and will likely follow up with a formal sleep study. This test, conducted while you sleep, measures brain and heart activity as well as the rate of breathing.
How Is Sleep Apnea Different Than Snoring?
Snoring may be a symptom of sleep apnea, but the two are different in a significant way. When a person snores, air has difficulty passing over the soft tissue somewhere along the airway. This could be in the nasal passages or throat. The soft tissue vibrates with the force of air, causing the sound we know as snoring.
When a person has sleep apnea, they stop breathing for moments at a time. Studies have indicated that a person with sleep apnea may stop breathing for several seconds before the brain releases adrenaline to restart respiration. These pauses in breathing can occur hundreds of times an hour.
What can Cause/Increase My Risk of Obstructive Sleep Apnea?
Sleep apnea can be a serious condition but it is one that can be managed and treated to reduce the short- and long-term effects of sleep loss and oxygen deprivation. Apnea episodes may increase or decrease with:
- Weight. Excessive weight causes the accumulation of fatty tissue around the airway. Patients are encouraged to lose weight if necessary and to maintain a healthy BMI.
- Alcohol and medications. Alcoholic beverages and sedatives such as sleeping pills, opioids, and other medications can cause muscles to relax to a point at which they interfere with breathing.
- Eating habits. People with sleep apnea are advised to avoid eating and consuming caffeine within two hours of going to sleep. Each of these can disrupt sleep.
- Sleep habits. The body is better able to properly relax and maintain a sleep cycle when a person maintains regular sleep hours, such as a 9 o’clock bedtime.
Some patients can minimize apnea episodes by sleeping with their head slightly elevated or sleeping on their side.
What are the non surgical treatment options?
- CPAP (Continuous Positive Airway Pressure).
- BiPAP (Bilevel Positive Airway Pressure).
- OA (Oral Appliance) Therapy.
What Are the Health Risks Associated with Untreated Sleep Apnea?

Untreated sleep apnea poses significant risks to overall health and well-being. When breathing stops intermittently during sleep, your body is deprived of oxygen, leading to serious health complications. Some of the most critical risks include:
- Cardiovascular Problems: Sleep apnea is closely linked with increased risk of high blood pressure, heart disease, and stroke. The recurrent oxygen drops cause blood pressure surges and strain the cardiovascular system.
- Type 2 Diabetes: Sleep apnea is a common comorbidity in people with type 2 diabetes, as the stress of frequent nighttime awakenings can influence glucose metabolism and increase insulin resistance.
- Metabolic Syndrome: This cluster of conditions, including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, is more prevalent in those with untreated sleep apnea.
- Liver Problems: People with sleep apnea are more likely to exhibit signs of liver function impairment and scarring (nonalcoholic fatty liver disease), which can progress to more severe liver damage over time.
- Mental Health Issues: Chronic sleep deprivation associated with sleep apnea can lead to depression, anxiety, and significant mood swings.
Clearly, addressing sleep apnea is crucial not just for improving sleep quality, but also mitigating these serious health risks.
Which Lifestyle Modifications Can Help Address Sleep Apnea?
Lifestyle changes can significantly impact the management of sleep apnea symptoms. Patients can adopt several strategies to minimize their symptoms:
- Weight Management: Since obesity is a major contributor to obstructive sleep apnea, losing weight can reduce the amount of fatty tissue in your throat, easing the airway obstruction during sleep.
- Sleep Position: Sleeping on your side can prevent your tongue and palate from falling backwards in your throat and blocking the airway. Special pillows and devices can help maintain a side sleeping position.
- Avoid Alcohol and Sedatives: These substances relax your throat muscles, which can worsen airway obstruction. Avoiding them can help reduce sleep apnea episodes.
- Quit Smoking: Smoking can increase inflammation and fluid retention in your airway, worsening sleep apnea.
- Regular Exercise: Besides aiding in weight management, regular exercise can improve sleep apnea by strengthening the muscles in your airway, making them less likely to collapse at night.
These lifestyle modifications are often the first line of defense against sleep apnea and can be highly effective in reducing symptoms and improving sleep quality.
Which Sleep Apnea Treatment Is Best?
CPAP (Continuous Positive Airway Pressure)
- Best for: Individuals with moderate to severe obstructive sleep apnea.
- How it works: CPAP devices use a hose connected to a mask or nosepiece to deliver constant and steady air pressure to help keep the airways open during sleep.
- Benefits: Highly effective in preventing airway closure during sleep, which reduces snoring and improves overall sleep quality.
BiPAP (Bilevel Positive Airway Pressure)
- Best for: Patients who have difficulty tolerating CPAP due to the constant air pressure, or those with central sleep apnea and coexisting obstructive sleep apnea.
- How it works: BiPAP provides two levels of pressure: higher when inhaling and lower when exhaling, making it easier for users who struggle with exhaling against a continuous pressure.
- Benefits: Especially useful for patients with cardiac or pulmonary disorders that make breathing difficult.
OA (Oral Appliance) Therapy
-
- Best for: Patients with mild to moderate obstructive sleep apnea who prefer a less intrusive option or cannot tolerate CPAP.
- How it works: Oral appliances adjust the position of the mouth and/or tongue to keep the airway open during sleep.
- Benefits: More portable and less cumbersome than CPAP, making them ideal for travel.
Each treatment option has unique advantages and considerations. Working closely with healthcare providers like Dr. Gould is important to find the most effective and comfortable treatment plan.
Schedule A Consultation
If you are suffering from sleep apnea in St. Louis or Festus, MO, please call 314-450-7720 to schedule a consultation with our experienced team at our office’s in St. Louis and Festus, MO. You can change your life with nose surgery and you can take the first step by speaking with us.